While most kids would feel anything but excited to see a school bus in July, Luckerly Gabriel could not wait to step on board. That is because this bus was headed to the Hole in the Wall Gang Camp, a specialized camp for youth with cancer and serious blood diseases. For Luckerly, he had been eager to go to camp for the past two years, and this summer he was finally healthy enough to do so. As a 10-year-old with sickle cell disease (SCD)—a chronic, genetic blood disorder which causes painful attacks and fatigue that can be especially difficult for kids—it had been a long time coming.
Shortly after moving to Boston from Haiti, Luckerly was experiencing severe pain caused by his disease and had to be hospitalized frequently. For Luckerly—and 100,000 other people, primarily of African descent, in the U.S. who have SCD—his red blood cells are shaped differently, like crescent moons, and are rigid and sticky. Because of this, the cells can become stuck together in tiny blood vessels which slows or blocks blood flow and oxygen. The result are episodes, or “crises,” of extreme pain in the chest, abdomen and joints lasting between a few hours to a few weeks. Cold weather can be especially difficult for people with SCD, because it can trigger painful crises. The effects of the trademark cold temperatures of New England winters on Luckerly’s health were an unexpected challenge for the family, who was already struggling with adjusting to a new language and culture. Luckerly’s family was eager to better understand his condition, so they transferred his care to Boston Medical Center’s Pediatric Sickle Cell Program. “Our Pediatric Sickle Cell Program provides outstanding care that is comprehensive and patient-focused, while providing families with the education required to help them understand this chronic disease,” notes Bob Vinci, MD, chairman of the Department of Pediatrics. “Our approach is multidisciplinary and innovative and looks at each patient individually with a goal of developing treatment programs that are best for each child and family.”
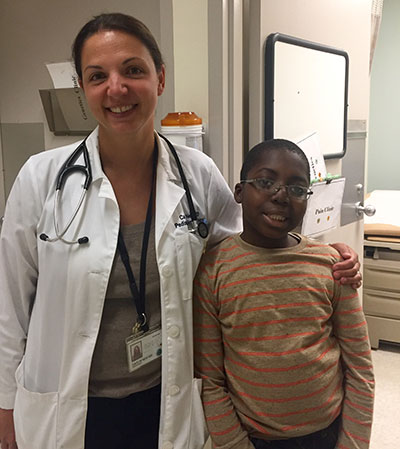
Caitlin Neri, MD, pediatric hematologist and oncologist and medical director of the Pediatric Pain Clinic, is part of Luckerly’s team of caregivers who implemented a treatment plan to better control his disease and prevent future hospitalizations. “We were able to help Luckerly by starting him on hydroxyurea, an excellent medication for sickle cell disease, which was not available in Haiti,” says Neri. “This has reduced the frequency of his pain episodes.” In addition to prescribing medication to help his condition, Luckerly’s team of providers helped him and his family adjust to life in a new country as best as possible. “We helped the family navigate the challenges of starting out in a new country, with lots of help from our pediatric hematology social worker, family navigator, Health Leads and other programs here at BMC,” adds Neri.
“BMC is great. My son was very sick, and the doctors were concerned about his [frequent episodes of pain] and so they focused on treating them. From the first time we came in, the care has been very good. They treat him very good.” – Luckerly’s mom
Two years into his care at BMC, Luckerly’s health has significantly improved and he experiences far fewer pain episodes, with severe episodes occurring about once per year. His team of providers continue to focus on a multidisciplinary approach to treating his SCD, which includes visits to the Pediatric Pain Clinic. “In Pain Clinic, Luckerly has access to both medical and non-medical therapies to manage pain,” explains Neri. “He has tried aromatherapy, acupressure and is learning mind-body strategies to help him cope with pain.” With Luckerly’s disease better controlled, BMC made sure he could experience activities that all 10-year-olds should, including summer camp. His caretakers coordinated all of the appropriate paperwork for his mom and before he knew it, he was on his way to a week of summer fun at the Hole in the Wall Gang Camp, along with 33 other children with SCD. “The week was specifically devoted to kids with SCD, and is instrumental in normalizing the disease for young patients, eliminating the barriers that frequently keep them from engaging in ‘normal’ kid activities and modeling proactive and effective disease management,” explains Child Life Specialist Ashley McClellan, CCLS. Luckerly returned from camp happier than ever, and could not wait to share his experiences with his mom. “He told me everything about camp, made friends and had a great time with them,” his mom recalls.
As Luckerly enjoys normal childhood activities, his family is deeply grateful to BMC for affording him with the ability to do so, never shying away from expressing their appreciation. “BMC is great. My son was very sick, and the doctors were concerned about his [frequent episodes of pain] and so they focused on treating them. From the first time we came in, the care has been very good,” concludes Luckerly’s mom. “They treat him very good.”